A 57 Year old female presented with Nausea, vomitings,. Fever , SOB
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent.
Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
A 57 YEAR OLD FEMALE WHO IS A RESIDENT OF YERRAVALLI CAME TO THE OPD WITH
CHIEF COMPLAINTS :
Vomitings since 5 days 1 episode per day
Fever since 5 days
Chest pain on and off since 3 days
SOB since 1 day
Cough with sputum
HISTORY OF PRESENT ILLNESS :
- Patient was apparently normal 5 days ago, Then she developed fever with chills and rigors, Nausea and vomitings 1 episode per day ( Non projectile, Non bilious, Content is of food particles).
- Pricking type of Abdominal pain with no aggravating or relieving factors
- 2-3 episodes of watery stools per day
- She then developed chest pain since 3 days along with back pain
- From yesterday she is having SOB, Cough with sputum and whole body weakness.
PAST HISTORY :
Diabetes - No
Hypertension - Present since 1 year ( un known medication)
TB - No
Asthma - No
Epilepsy - No
CVD - No
Chemo/Radiation Exposure - No
Surgical history - Total abdominal hysterectomy 15 years ago
FAMILY HISTORY : Nil significant
PERSONEL HISTORY :
Diet - Mixed
Appetite - Lost since 5 days
Bowel movements - Watery stools
Bladder movements - Normal
Allergies - No
Addictions - No
GENERAL EXAMINATION :
Temperature - 96.9 °F
Pulse - 90 beats/min
BP - 120/80 mmHg
RR - cycles/min
GRBS - mg%
SPO2 - 100 %
Pallor - No
Icterus - No
Clubbing - No
Cyanosis - No
Lymphadenopathy - No
SYSTEMIC EXAMINATION :
CVS :
No thrills
No murmurs
S1 and S2 heard
RESPIRATORY SYSTEM :
Position of trachea - Central
No Dyspnoea , Wheeze
Breath Sounds - vesicular
ABDOMEN :
Shape - Scaphoid
No Tenderness
No palpable mass
Umbilicus inverted
Bowel sounds heard
CNS : Normal
- Patient is Consious, Coherent, Well oriented to time place and surroundings.
INVESTIGATIONS :
1/9/22 -
Serum Creatinine:
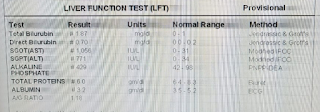
LFT :
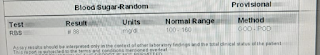
Random blood sugar :
Serum Electrolytes:
PROVISIONAL DIAGNOSIS :
Dengue with severe thrombocytopenia
TREATMENT :
- IV fluids NS
RL @ 100ml/hr
- Inj Optineuron 1amp in 100 ml IV/OD
- Inj Pan 40 mg IV/OD
- Inj Zofer 4 mg IV /SOS
- TAB Dolo 650 mg TID
- Inj Doxy 100 mg IV/BD
- Inj Neomol 1mg IV/SOS
- Strict I/O Charting
- W/F Bleeding manifestation
- Monitor vitals and inform SOS










Comments
Post a Comment