A 14 year old girl presented with fever and cough
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent.
Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
A 14 year girl who is a resident of Chinnathummala came with chief complaints of
CHIEF COMPLAINTS :
- Fever for 3 days 5 days back
- Cough with sputum since yesterday
HISTORY OF PRESENT ILLNESS :
- Patient was apparently normal 7 days back then she developed low grade fever for 3 days which increased at night not associated with chills and rigors. Then she went to a private hospital and found to have low Haemoglobin( 3.38 gm/dl) and platelet count.
- After 5 days she had cough with sputum white in colour non blood stained since yesterday night
- No H/o Nausea, Vomiting, weight loss, Abdominal pain, Giddiness, Headache.
PAST HISTORY :
Diabetes - No
Hypertension - No
TB - No
Asthma - No
Epilepsy - No
CVD - No
Chemo/Radiation Exposure - No
Surgical history - No
FAMILY HISTORY : Nil significant
MENSTRUAL HISTORY:
Age of menarche - 12 years
Cycles are regular, 30 days cycle
Flow is Normal ( 5 days ), 2-3 pads per day
Not associated with pain and clots
PERSONEL HISTORY :
Occupation - Student(7th class)
Diet - Mixed
Appetite - Normal
Bowel and bladder movements - Regular
Allergies - No
Addictions - No
GENERAL EXAMINATION :
Temperature - Afebrile
Pulse - 77 beats/min
BP - 120/90 mmHg
RR - cycles/min
GRBS - 106 mg%
SPO2 - 100 %
Pallor - Present
Icterus - No
Clubbing - No
Cyanosis - No
Lymphadenopathy - No
SYSTEMIC EXAMINATION :
CVS :
No thrills
No murmurs
S1 and S2 heard
RESPIRATORY SYSTEM :
Position of trachea - Central
No Dyspnoea , Wheeze
Breath Sounds - vesicular
ABDOMEN :
Shape - Scaphoid
No Tenderness
No palpable mass
Umbilicus inverted
Bowel sounds heard
CNS : Normal
Patient is Consious, Coherent, Well oriented to time place and surroundings.
INVESTIGATIONS :
25/8/22:
Blood grouping and Rh typing- O positive
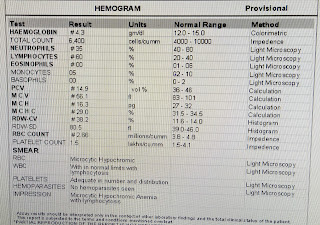
Haemogram -
26/8/22 :
Random blood sugar - 91 mg/dl
Blood urea - 15 mg/dl
CRP - Negative
ESR - 85 mm 1st hour
LDH - 212 IU/L
Reticulocyte count - 0.9 %
Serum Creatinine - 0.4 mg/dl
Serum iron - 64 ug/dl
CUE -
LFT -
Serum Electrolytes -
28/8/22 :
Haemogram -
29/8/22 :
Haemogram -
PROVISIONAL DIAGNOSIS :
Severe Anaemia with decreased evaluation.
TREATMENT :
27/8/22 -
Monitor vitals
Inj Optineuron in 100 ml NS over 30 min IV/OD
O/E : Patient is c/c/c
BP - 100/70 mmHg
PR- 80 bpm
RR- 18 cpm
SPO2 - 100% on RA
CVS - S1,S2 Heard
R/S - BAE +
P/A - Soft, Non tender.
28/8/22 -
Monitor vitals
Inj Optineuron in 100 ml NS over 30 min IV/OD
Inj Iron sucrose 200 mg/IV in 100ml NS slow over 1 hour
O/E : Patient is c/c/c
BP - 100/70 mmHg
PR- 70 bpm
RR- 14 cpm
Temp - 97°F
CVS - S1,S2 Heard
R/S - BAE +
P/A - Soft, Non tender.
29/8/22 -
Monitor vitals
Inj Iron Sucrose 100mg in 100ml NS alternate day
O/E : Patient is c/c/c
BP - 110/70 mmHg
PR- 70 bpm
Temp - 98.6°F
SPO2 - 100% on RA
CVS - S1,S2 Heard
R/S - BAE +
P/A - Soft, Non tender.









Comments
Post a Comment