VIRAL PYREXIA
Saturday, December 18, 2021
A CASE OF 45 YEAR OLD FEMALE PATIENT WITH SOB, FEVER, PAIN ABDOMEN AND GENERALISED WEAKNESS.
A 45 year old female came to the OPD with the C/O Fever since 3 days
HOPI :
Patient came with c/o fever since 10 days
Generalised body pains since 10 days
Pain abdomen since 5 days
History of presenting illness :
Patient was apparently normal ten days back then she developed fever , low grade associated with chills and rigors not associated with cough, no burning micturition , no vomiting , no loose stools. Fever subsided after medication 5 days back.
Then, since 5 days patient developed pain abdomen around umbilicus and epigastrium, non radiating associated with SOB grade 3 and 4 , not associated with nausea and vomiting , loss of appetite .
History of past illness :
Not a K/C/O HTN/DM/TB/Epilepsy/Asthma/CAD/CVA
Patient was hysterectomised 15 years ago.
Family history - Not Significant
Personal History :
Diet- mixed
Appetite- normal
Sleep- adequate
Bowel and bladder movements- regular
No addictions
General Examination :
Patient is Consious , Coherent , Cooperative.
No pallor , icterus , cyanosis , clubbing , koilonychia , lymphadenopathy , edema.
Vitals at admission :
Temp - 100 F
PR- 120 bpm
BP- 90/60 mmHg
RR- 40 cpm
SpO2- 97% at RA
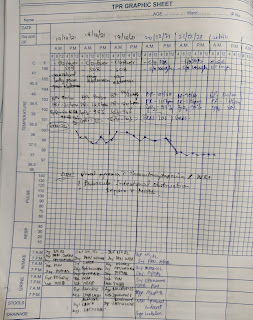
Fever chart:
Systemic Examination :
CVS - S1 S2 heard , no murmurs
RS - BAE+ , B/L IAA, IMA crepts
CNS - NAD
P/A - Soft, Non tender
Provisional diagnosis :
Viral Pyrexia with Thrombocytopenia, viral pneumonia, sepsis with MODS.
Investigations on admission :
CUE :
Albumin +
Ec : 2 to 3 cells
Puss cells : 3 to 4 cells
Blood Sugar : negative
BP: negative
Sugar : negative
Blood cells and casts : negative
Blood urea : 90 mg/dl
Serum creatinine : 1.1 mg/dl
Na+ : 139
K+ : 4.8
Cl- : 95
LFT :
TB : 7.01 mg/dl
DB : 3.10 mg/dl
AST : 111 IU/L
ALT : 75 IU/L
ALP : 403 IU/L
TP : 6.3 mg/dl
ALBUMIN : 2.0 mg/dl
ABG :
PH: 7.37
PCO2 : 53.3
PO2 : 38.1
HCO3- :30.3
ST. HCO3- : 26.7
Other investigations :
Myeloperoxidase : Negative
HIV : Negative
HBsAg : negative
HCV : negative
RAPID DENGUE : negative
RT-PCR : negative
ECG :
2D ECHO :
USG :
X RAY :
ECG on 18/12/21
Review USG :
Investigations on 19/12/21
Hb: 9.3
Tlc: 20,800
Plt. Count : 3.73
Serum total bilirubin: 9.92 mg/dl
Direct bilirubin: 3.21 mg/dl
Serum creatinine : 0.7 mg/dl
X Ray -
Plan of treatment
1. Ivf NS/RL/DNS continuous at 100ml/hr
2. Inj. PAN 40mg IV BD
3. inj. ZOFER 4mg IV/SOS
4. Inj. NEOMOL 1gm IV/SOS
5. Inj. PIPTAZ 4.5 gm IV TID
6. Tab. PCM 650 mg PO/ SOS
7. Inj. OPTINEURON 1 AMP in 100ml NS IV/OD
8 Tab. TUSQ 1 tab PO BD
9. SYP. ASCORYL-LS 10ml PO TID
10. NEB. IPRAVENT 6th hourly
NEB. BUDECORT 12th hourly
11. BP/PR/TEMP monitoring 4th hourly
12. GRBS charting 12th hourly.
13. Intermittent CPAP if not maintaining on O2
14. Syp. LACTULOSE 10 ml PO TID
20/12/21
Investigations :
CRP -
Treatment :
1. Ivf NS/RL continuous at 75 ml/hr
2. Inj. PAN 40mg IV OD
3. inj. ZOFER 4mg IV/SOS
4. Inj. NEOMOL 1gm IV/SOS if temp >102 F
5. Inj. PIPTAZ 4.5 gm IV TID
6. Tab. PCM 650 mg PO/ TID
7. Inj. OPTINEURON 1 AMP in 100ml NS IV/OD
8 Tab. TUSQ 1 tab PO BD
9. SYP. ASCORYL-LS 10ml PO TID
10. NEB. IPRAVENT 6th hourly
NEB. BUDECORT 12th hourly
11. BP/PR/TEMP monitoring 4th hourly
12. GRBS charting 12th hourly.
13. Intermittent CPAP if not maintaining on O2
14. Syp. LACTULOSE 10 ml PO TID
15. Tab Azithromycin 500mg PO/OD
16. Tal Udiuvi 300mg PO/BD
17. Inj Hydrocort 100mg IV/BD
21/12/21
Investigations :
Haemogram -
Fever chart -
Treatment :
1. Ivf NS/RL/DNS continuous at 70 ml/hr
2. Inj . PIPTAZ 4.5 gm IV TID
3.. Inj. PAN 40mg IV BD
4. inj. ZOFER 4mg IV/TID
5.Inj. NEOMOL 1gm IV/SOS
6. Tab. PCM 650 mg PO/ SO
7. Inj. OPTINEURON 1 AMP in 100ml NS IV/OD
8 Tab. TUSQ 1 tab PO BD
9. SYP. ASCORYL-LS 10ml PO TID
10. NEB. IPRAVENT 6th hourly
NEB. BUDECORT 12th hourly
11. Inj . HYDROCART 100 mg BD
12. Syp LACTULOSE 20 ml HIS
22/12/21
LFT





















Comments
Post a Comment